Emma Morris // October 16, 2020 // Updated: February 18, 2021
Originally Posted at OKPolicy.org
Following voters’ approval of Medicaid expansion during the June 30 election, Oklahoma’s next steps should be relatively simple. The state has already been providing high-quality, low-cost Medicaid for years; the Oklahoma Health Care Authority (OHCA) has a decades-long track record of excellence in efficiency and effectiveness. OHCA could expand Medicaid to cover more than 200,000 low-income Oklahomans for between $125 million and $164 million, all without raising taxes.
Unfortunately, Gov. Stitt and OHCA CEO Kevin Corbett have unilaterally decided that after decades of proven results, Oklahoma should try something else, something that has never worked in the state, and something that, if other states’ experiences hold true here, will cost the state much more money than in-house expansion. Their proposal for managed care, though appealing in the abstract, harkens back to Oklahoma’s previous failed attempt at a similar plan. To avoid unnecessary cuts to provider rates or medical services, Oklahoma must ensure that Medicaid administration remains in the proven, capable hands of the Oklahoma Health Care Authority.
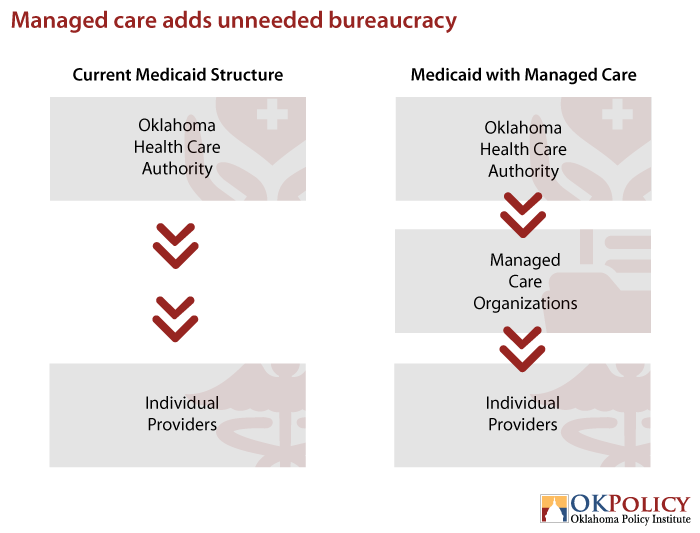
Managed care adds an unneeded layer bureaucracy to Oklahoma’s Medicaid program
Simply put, transitioning to managed care would outsource the services that OHCA already provides. Currently, most Oklahoma Medicaid enrollees are served through SoonerCare Choice, meaning that OHCA contracts directly with primary care providers to coordinate patient care. In the capitated managed care model proposed for Oklahoma, state Medicaid agencies contract with privately owned managed care organizations (MCOs), who then contract with providers to coordinate care. States pay the MCOs a monthly per-member capitation payment. If the MCO can provide services for less than the monthly payment, it makes a profit. If not, the MCO loses money.
Gov. Stitt has championed minimizing bureaucracy throughout his time in office, so it’s difficult to understand the reason for adding an additional management layer. Perhaps this would make more sense if managed care had historically been cheaper than the in-house SoonerCare Choice model, but that’s not the case either. SoonerCare Choice boasts lower administrative costs than most states with managed care, and a national study has already found that “with sufficient resources and leadership commitment, state Medicaid agencies can manage care at lower costs than managed care organizations and with similar outcomes.”
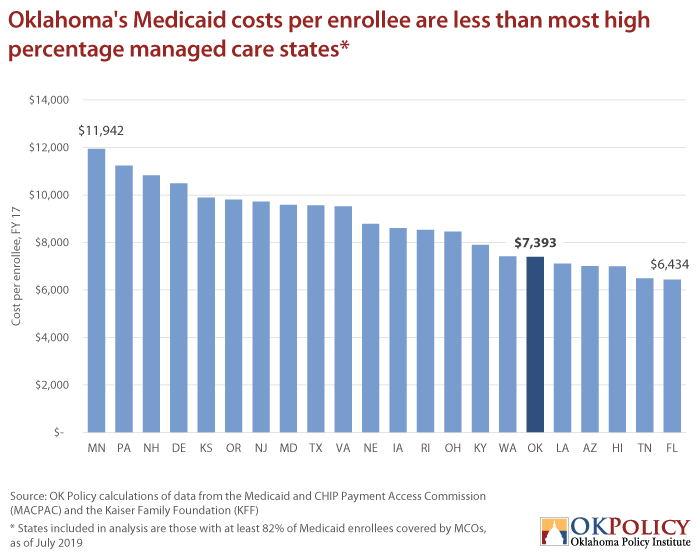
Oklahoma does not have the problems that managed care is supposed to fix. States often privatize Medicaid in hopes of reducing “haphazard care,” maintaining budget stability, and decreasing Medicaid costs. The majority of care in Oklahoma, however, is already coordinated through SoonerCare Choice, and Oklahoma’s cost per Medicaid enrollee is already lower than most other states. No compelling evidence suggests that implementing managed care would lower cost in Oklahoma.
Managed care could cost the state more money
There is no definitive evidence that managed care brings savings for the state; indeed, most studies have found that managed care tends to be either cost neutral or more expensive. Managed care organizations must make a profit to survive, and those billions in profit come directly from taxpayers. In the midst of the coming state budget crisis, taxpayer dollars must be used to fund existing services, not funneled to private corporations. In Oklahoma, savings are unlikely because of potential MCO demands for rate increases, Oklahoma’s already low administrative costs, and comparatively low costs per enrollee, and the potential loss of federal funds.
Budget stability is far from a guarantee. As demonstrated by other states, as well as Oklahoma’s first foray into managed care, MCOs are known to demand significant rate increases. Because of Oklahoma’s weak MCO market, this could easily leave the state scrounging for more money to maintain existing services.
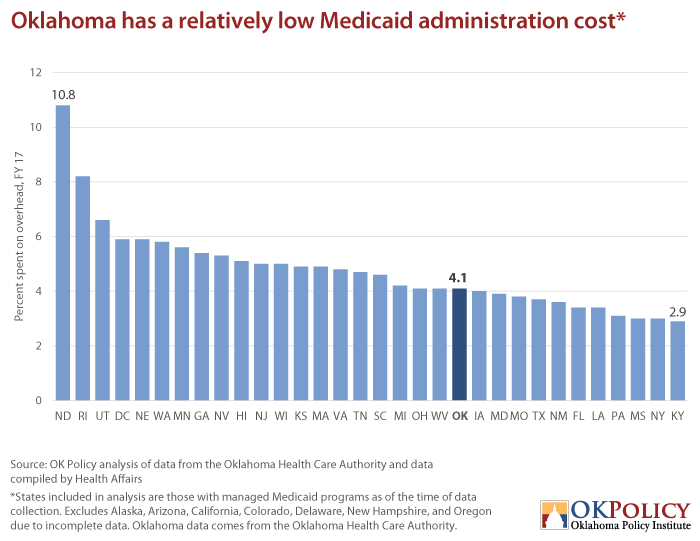
Additionally, Oklahoma already has a low Medicaid administrative cost, with only 3.7 percent of expenses going to overhead administration in 2019. That number has even decreased in recent years; in 2017, administration accounted for just 4.05 percent of total SoonerCare expenditures, which was less than the administrative costs in most states that used managed care (shown in the graph below). In rural areas, managed care organizations find it difficult to achieve increased administrative savings due to the need for in-house services for rural residents. Oklahoma will certainly have to account for this need because outsourced care coordination has already proven unfeasible in rural Oklahoma.
While inclusion of the expansion population in privatized managed care will likely decrease Oklahoma’s overall cost per enrollee, medical costs could easily increase. In 2019, Oklahoma spent $7,393 per Medicaid enrollee, the lowest of states in the surrounding region that had not expanded Medicaid (Kansas, Missouri, and Texas). These states rely heavily on managed care organizations, and recorded costs per enrollee between $9,558 and $12,065 with an average cost of $10,503. If Oklahoma’s per-person costs increased to that average, SoonerCare could have cost the state an additional $716 million. As shown in the graph below, Oklahoma’s per-enrollee cost is also already less than that of most states nationwide with high managed care usage.
Lastly, implementing managed care could lead to a significant loss of federal funds. Services provided for American Indians through Indian Health Care Providers (IHCPs) are currently reimbursed by the federal government at a rate of 100 percent, according to a recent Senate interim study. If the state shifts to managed care, it could lose the 100 percent matching rate for some services provided to American Indians through managed care organizations, meaning that available federal funds would remain in Washington, leaving Oklahoma to foot the entire bill.
We’ve been down this road before…and it didn’t work
Managed care has a history of poor performance in Oklahoma, and there’s no evidence to suggest the market has changed in recent years. In the 1990s, managed care was only feasible in urban areas, and many providers were reluctant to enter into contracts. A 2003 demand from MCOs for an 18 percent rate increase — and subsequent realizations that OHCA could administer the program for a quarter of the cost — drove the nail into the coffin of Oklahoma’s first attempt. A 2015 bill passed by the Legislaturedirected OHCA to explore managed care, and this attempt was again abandoned to avoid cuts to provider rates.
Taxpayers deserve a fiscally responsible Medicaid program that prioritizes patient needs. OHCA has already proven that it can administer Medicaid for a lower cost than managed care organizations, with fewer staff and less bureaucracy. Medicaid privatization has yet to work in Oklahoma, and taxpayer money shouldn’t be used for another experiment.